Is Alcohol Off Limits? How Drinking Affects Diabetic Balance
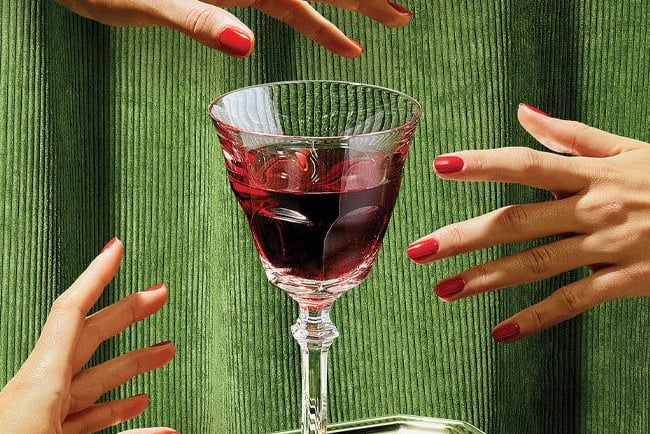
Many of us enjoy unwinding with a glass of wine or beer in good company from time to time. But what if you have diabetes? Does the diagnosis mean giving up alcohol entirely? Let's explore how alcohol affects blood sugar levels and whether it's possible to strike a balance between caution and a fulfilling social life.
DIABETES
Written by Laura Felute, MS, RDN
5/22/20253 min read

The Complex Dance: How Alcohol Affects Glucose Metabolism
Alcohol's relationship with blood sugar in people with diabetes is paradoxical. Initially, many alcoholic beverages can spike glucose levels due to their carbohydrate content—think sweet cocktails or beer. However, the real danger lurks in what happens next.
Hours after your last sip, there's a significant risk of blood sugar plummeting dangerously low. This occurs because your liver becomes preoccupied with processing alcohol, temporarily abandoning its crucial role of releasing stored glucose into your bloodstream. The window between 2 and 8 AM becomes particularly treacherous—a time when hypoglycemia risk peaks while you're likely asleep and unable to respond.
What makes this especially dangerous is alcohol's ability to mask hypoglycemia symptoms. That dizziness, slurred speech, and unsteady gait? Others (and you yourself) might dismiss these as typical intoxication rather than recognizing them as warning signs of a medical emergency.
Here's a sobering fact: your body metabolizes roughly one standard drink per hour, but alcohol's effects on glucose regulation can persist for up to 24 hours after consumption.
Smart Strategies for Safe Social Drinking
If you have diabetes and choose to drink, these evidence-based strategies can help minimize risks:
Never drink on an empty stomach. Always eat a substantial meal containing protein, healthy fats, and complex carbohydrates before consuming alcohol. This combination slows alcohol absorption and helps stabilize blood sugar levels.
Become a glucose monitoring champion. Check your blood sugar before drinking, periodically during consumption, and especially before bedtime. If your reading drops below 5,6 mmol/L at bedtime, consume an additional protein-rich snack.
Choose your poison wisely. Opt for beverages with minimal carbohydrate content: dry wines, brut champagne, or spirits mixed with sugar-free beverages (like vodka with club soda) are safer bets than sugary cocktails or regular beer.
Embrace moderation. The general guideline suggests one standard drink daily for women and two for men, with several alcohol-free days each week.
Pace yourself deliberately. Alternate each alcoholic drink with water and savor each beverage slowly—make one drink last an hour.
Create a support network. Ensure those around you understand your condition and can recognize hypoglycemia symptoms.
Carry emergency supplies. Keep glucose tablets, juice, or hard candy readily available for rapid blood sugar correction.
Debunking Common Myths
Myth 1: "Sugar-free drinks like dry wine and vodka are completely safe for diabetics" Reality: Even zero-sugar beverages can trigger dangerous glucose drops due to alcohol's impact on liver function. The alcohol content itself matters more than sugar content.
Myth 2: "Extra insulin compensates for sweet cocktails" Reality: This approach is dangerously flawed. Both insulin and alcohol lower blood sugar, creating unpredictable interactions. Alcohol also alters insulin absorption rates, making dosage calculations nearly impossible.
Myth 3: "Diabetes means absolute alcohol prohibition" Reality: For most people with well-controlled diabetes, moderate consumption is acceptable when proper precautions are taken. However, certain medical conditions do require complete abstinence.
Myth 4: "Light beer is the diabetic's best friend" Reality: Even light beer contains carbohydrates from malt that can affect blood sugar. The "light" refers to calories, not carbs.
Myth 5: "Feeling fine means everything's okay" Reality: Alcohol masks hypoglycemia symptoms, and dangerous effects often emerge hours later, potentially while you're sleeping.
Essential Questions Answered
How can I distinguish hypoglycemia from intoxication? While symptoms overlap, hypoglycemia typically includes intense hunger, hand tremors, profuse sweating, and rapid heartbeat—symptoms rarely associated with simple intoxication. When in doubt, check your glucose or assume hypoglycemia and consume fast-acting carbohydrates.
When is hypoglycemia risk highest after drinking? Peak danger occurs 8-12 hours post-consumption, often during sleep or early morning hours. This timing makes bedtime glucose monitoring and strategic snacking crucial, even with normal readings.
How does regular drinking affect long-term diabetes management? Consistent alcohol consumption can elevate HbA1c levels by 0.3-0.5% in people with type 2 diabetes while potentially reducing the effectiveness of glucose-lowering medications and insulin.
Finding Your Personal Balance
Diabetes doesn't automatically eliminate alcohol from your life, but it demands a thoughtful, science-based approach. The cornerstones of safety remain moderation, strategic planning, and vigilant monitoring.
Ultimately, the choice to drink with diabetes is deeply personal and should be made in consultation with your healthcare team. For many people with diabetes, moderate alcohol consumption can coexist with both effective disease management and a rich social life—provided you approach it with knowledge, preparation, and respect for your body's unique needs.
Your health must always take precedence, and sometimes that means saying no to alcohol in certain situations or entirely. However, with proper education and careful strategies, you can make informed decisions that preserve both your wellbeing and your quality of life while successfully managing diabetes.
Wellness
Empowering health through personalized care solutions.
Care
Health
© 2025 Care Health Wellness. All Rights Reserved. Web Design and Digital Marketing by Webartline
